Article Summary
Increased risk of cardiometabolic comorbidities in patients with adrenal incidentalomas with and without autonomous cortisol secretion
Yasir Elhassan, Fares Alahdab, Alessandro Prete, et al. Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess: a systemic review and meta-analysis. Ann Intern Med. 2019;171(2):107-116. doi:10.7326/M18-3630
Incidental detection of adrenal masses has increased due to the use of cross-sectional imaging. These adrenal incidentalomas are found in approximately 5% of patients, with increasing incidence by age. Most adrenal incidentalomas are benign, nonfunctioning adrenal tumors (NFATs), but up to 15% are associated with excess hormone secretion. These secretory adenomas are often associated with autonomous cortisol secretion, a condition characterized by elevated levels of cortisol without the typical physical changes associated with hypercortisolism.* A better understanding of the natural history of these two adenoma types is required to determine appropriate management and follow-up plans for both NFATs and autonomous cortisol secretion.
To determine the natural history of adrenal incidentalomas, a systematic review and meta-analysis analyzed 32 studies reporting the outcomes of 4121 patients with NFAT or autonomous cortisol secretion.† Specific outcomes of interest included adenoma growth, changes in hormone production, the frequency of cardiovascular and metabolic comorbidities‡ between baseline and follow-up, and all-cause and cardiovascular mortality.
The meta-analysis showed that patients with autonomous cortisol secretion had a higher prevalence of cardiovascular risk factors at baseline and were more likely to develop or show worsening of these factors during follow-up than patients with NFAT. Additionally, patients with NFATs were at elevated risk for type 2 diabetes and cardiovascular comorbidities relative to patients without any adrenal adenomas. Although adenoma growth and changes in hormonal function were relatively stable over time, the meta-analysis concluded that clinical follow-up is warranted for patients with NFAT or autonomous cortisol secretion due to their increased risk for cardiometabolic comorbidities.
This summary uses the term autonomous cortisol secretion to conform with the nomenclature used by the American Association of Clinical Endocrinologists (AACE). According to the AACE, an incidentally discovered adrenal mass with a 1-mg post-dexamethasone suppression test (DST) >1.8 μg/dL may indicate autonomous cortisol secretion. For more information, see Vaidya A, Hamrahian A, Bancos I, Fleseriu M, Ghayee HK. The evaluation of incidentally discovered adrenal masses. Endocr Pract. 2019;25(2):178-192.
†Definition criteria for autonomous cortisol secretion varied across studies and included DST cortisol cutoff thresholds ranging from 1.8 to 5 μg/dL.
‡Cardiovascular and metabolic comorbidities included hypertension, obesity or weight gain, dyslipidemia, type 2 diabetes, and cardiovascular events.
Adrenal incidentalomas exhibited minimal growth and no malignancy at follow-up
6.3% of 3043 patients with NFAT or autonomous cortisol secretion demonstrated some degree of tumor growth at follow-up (mean follow-up duration: 41.9 months)
In studies that reported tumor size at baseline, there was no difference in tumor growth between patients with NFAT and patients with autonomous cortisol secretion (2 mm mean increase with a mean follow-up duration of 52.8 months; n=1105; 95% CI, 1 to 3 mm)
Tumor size increases of ≥10 mm were reported in 2.5% (CI: 1.8-3.3) of 2023 patients at follow-up* (mean follow-up duration: 41.5 months)
Tumor growth was more likely to occur in patients with autonomous cortisol secretion [2.4% (CI: 0.0-9.6); n=55] than in patients with NFAT [1.2% (CI: 0.5-2.0), n=1088]
No adrenal adenomas transformed into malignant tumors during follow-up [mean follow-up duration: 49.3 months (range, 1 to 204 months); n=2854]
CI, confidence interval.
Shorter follow-up durations (<12 months) were associated with fewer growths larger than 10 mm compared with longer follow-up durations (≥24 months).
Hormone production by adrenal incidentalomas was relatively stable over time
Progression of NFATs over time

†The likelihood of developing autonomous cortisol secretion was consistent across varying DST cortisol cutoff values.
- Only 6 of 2,745 patients with NFAT or autonomous cortisol secretion at baseline developed overt Cushing syndrome at follow-up (mean follow-up duration: 49.6 months)
- Few patients with autonomous cortisol secretion (18 of 840) experienced resolution of cortisol excess at the time of follow-up‡ (mean follow-up duration: 49.8 months)
‡The likelihood of autonomous cortisol secretion resolution was slightly lower in studies using a DST cortisol cutoff of 5 μg/dL.
Both NFAT and autonomous cortisol secretion were associated with a high prevalence of cardiometabolic conditions
At Baseline
- Patients with NFAT or autonomous cortisol secretion demonstrated a high prevalence of hypertension, obesity, dyslipidemia, and type 2 diabetes at baseline (60%, 42%, 33.7%, and 18.1% of patients, respectively)
Comorbid Condition(s) at Baseline

At Follow-Up
Comorbidities were more likely to develop and worsen in patients with autonomous cortisol secretion than in those with NFAT.
Compared with the NFAT group, patients with autonomous cortisol secretion were more than twice as likely to gain weight (21% vs 8.7%, respectively).
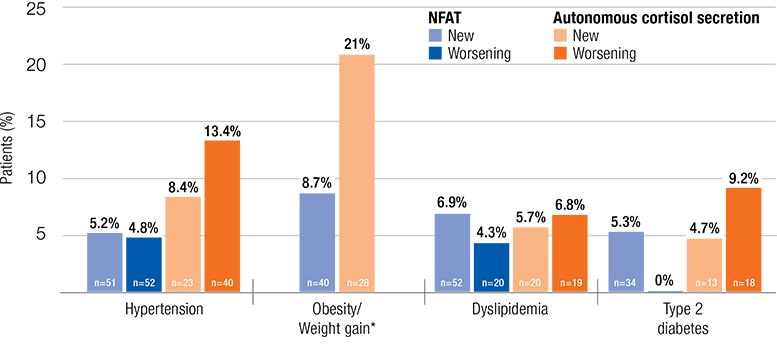
Data on worsening of obesity/weight gain were not included in the meta-analysis.
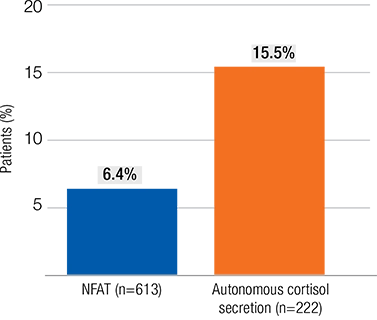
Patients with autonomous cortisol secretion demonstrated higher numbers of new cardiovascular events
Patients with autonomous cortisol secretion were twice as likely to experience a new cardiovascular event (15.5% vs 6.4%, respectively) than patients with NFATs.
- All-cause mortality was similar between patients with NFAT and those with autonomous cortisol secretion and was relatively high across studies (11.2%; mean follow-up duration: 56.3 months; n=1,356)
- None of the included studies had an ideal follow-up duration for assessment of mortality rates
- Cardiovascular mortality was also similar between the NFAT and the autonomous cortisol secretion groups and represented 43% of all study deaths
Patients Experiencing a New Cardiovascular Event